Coronavirus September 2022—Part 16 Should You Get a Bivalent Booster Shot?
In this post, we explore the pros and cons of getting a bivalent booster shot against COVID-19. As usual, if you’re less interested in how we got to our conclusions than you are in the conclusions themselves, feel free to skip to the CONCLUSION at the end.
Question: Should you get a bivalent booster shot?
Answer: It depends, again, on how likely you are to have a bad outcome if you contract COVID-19 as well as your specific goals in getting vaccinated.
THE EVIDENCE
Unfortunately, the evidence that argues that there’s a benefit to receiving a bivalent booster is quite weak. As of this writing, there exists no data on human subjects. All data on both the Moderna and Pfizer bivalent boosters have come from studies in mice. Further, the only outcomes that have been measured are neutralizing antibody responses. Here are the reasons this is problematic:
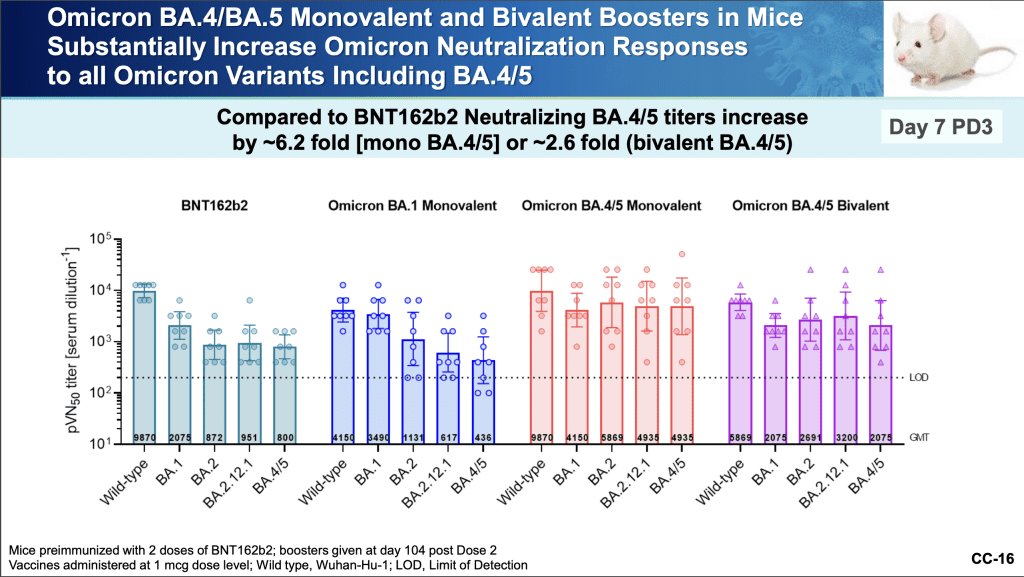
- We don’t know how long these elevated levels of neutralizing antibodies will last. High levels of neutralizing antibodies do correlate with resistance to infection. However, studies show (here and here) that neutralizing antibodies decline rapidly within three months of COVID immunization and though they continue to decline at a slower rate thereafter, they end up substantially lower at the six-month mark. (This seems to be an unfortunate feature of immunization against COVID specifically; for example, when people are vaccinated against measles, mumps, and rubella, neutralizing antibodies drop at a rate of only 5 – 10 percent per year.) Interestingly, people who’ve been vaccinated and infected—who have what’s termed hybrid immunity—show a much slower rate of neutralizing antibody decay, dropping only modestly 8 to 10 months after infection. Curiously, in the mouse Pfizer study, the preparation that generated the highest level of neutralizing antibodies was not the bivalent booster (the booster designed to produce antibodies both to the original COVID variant and the BA.4 and BA.5 variants). It was the monovalent booster (the booster designed only to produce antibodies to BA.4 and BA.5). In fact, the monovalent booster induced a concentration of neutralizing antibodies to the BA.4 and BA.5 variants that was as much above that induced by the bivalent booster as the concentration induced by the bivalent booster was above the original vaccine! (See chart below.) Why Pfizer has chosen to roll out the bivalent booster when as of this writing more than 95 percent of circulating COVID in the U.S. is currently either BA.4 or BA.5 remains unclear.
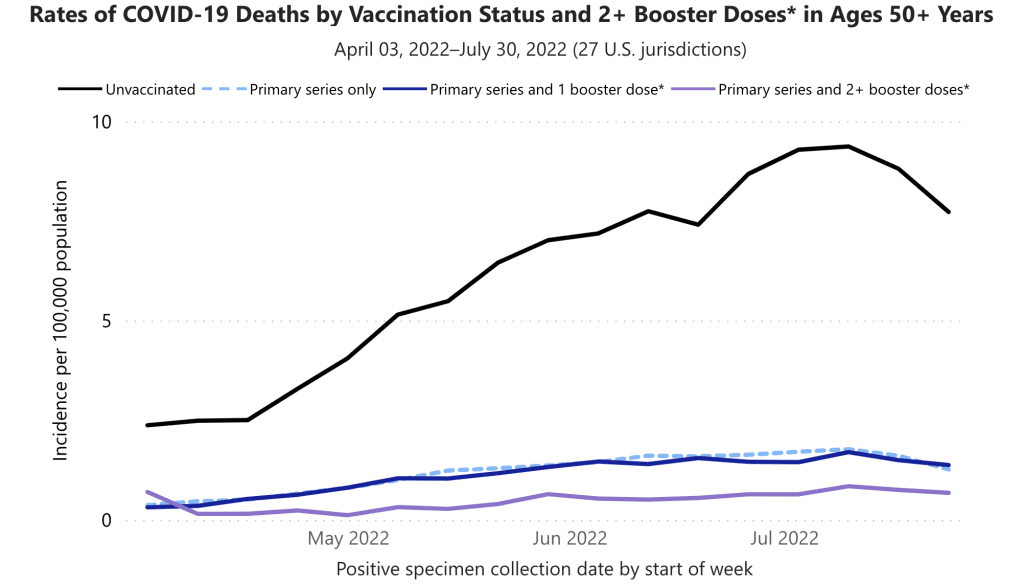
- We don’t know if the bivalent booster will further reduce the already low rate of death gained from just 2-3 shots. As of this writing, if you received just the primary series (two shots) or the primary immunization series and one booster dose, the incidence of death from COVID is almost identical at about 1.3 people per 100,000 (see graph below). The incidence of death from COVID if you received the primary immunization series and two booster doses is 0.68 people per 100,000 (see graph below). The absolute difference in the incidence of death between three shots vs. four shots is 0.62 people per 100,000. (Note that these numbers don’t indicate the actual risk of dying if you get COVID. To calculate that, we’d need to have accurate data for the number of COVID cases, which, given that most COVID is now diagnosed at home with rapid antigen tests and not reported, we don’t have.) The reason, however, that the rate of death in the population from COVID is now so low is that all the COVID vaccines induce cellular immunity responses—B cell and T cell responses—that over long periods of time (likely over our entire lifetimes) remain robust enough to curtail serious infection.
While being immunized may reduce the risk of some forms of long COVID, we have no data to suggest that immunizing beyond the primary series further reduces the risk of long COVID. More studies are needed. Human trials of both Moderna’s and Pfizer’s bivalent boosters are underway, but we won’t have the results for many months yet.
CONCLUSION: Should you get the bivalent booster? In the absence of human trial data, we might think about this question as follows: We can be reasonably certain that the bivalent booster will produce a level of neutralizing antibodies that diminishes the risk of infection from COVID. We don’t know how long that protection will last, but a fair guess would be from 3 to 6 months. If there is some reason you feel the need to reduce your risk over the next 3 to 6 months, say, for travel, getting the bivalent booster would seem reasonable. On the other hand, if in addition to being vaccinated, you’ve had COVID recently (meaning you’ve been infected with an Omicron variant), likely the same level of protection accrues, obviating the need for the bivalent booster. If your main concern is dying from COVID and you’ve already received the primary series and one or two boosters, your risk is so low that getting another shot would seem superfluous. If you are at high risk for dying from COVID, while there is no data to suggest the bivalent booster might further reduce your risk beyond levels afforded by the primary series and one or two boosters, there is also likely little risk of getting it. In the absence of data to guide us, this would then be a personal decision.
- Coronavirus February 2020—Part 1 What We Know So Far
- Coronavirus March 2020—Part 2 Measures to Protect Yourself
- Supporting Employee Health During the Coronavirus Pandemic
- Coronavirus March 2020—Part 3 Symptoms and Risks
- Coronavirus March 2020—Part 4 The Truth about Hydroxychloroquine
- Coronavirus April 2020—Part 5 The Real Risk of Death
- Coronavirus April 2020—Part 6 Evaluating Diagnostic Tests
- Coronavirus April 2020—Part 7 The Accuracy of Our Antibody Test
- Coronavirus May 2020—Part 8 How to Reopen a Business Safely
- Coronavirus August 2020—Part 9 Masks, Vaccines, and Rapid Testing
- Coronavirus December 2020—Part 10 Should You Get the Pfizer Vaccine?
- Coronavirus December 2020—Part 11 Should You Get the Moderna Vaccine?
- Coronavirus April 2021—Part 12 Should You Get the Johnson & Johnson Vaccine?
- Coronavirus May 2021—Part 13 How Effective are the Vaccines in the Real World?
- Coronavirus August 2021—Part 14 The Delta Variant, Masks, and Vaccines
- Coronavirus October 2021—Part 15 Should You Get a Third Booster Shot?