Direct Primary Care Being Offered by a Hospital System?
I recently had an interesting conversation with a long-time benefit consultant that got me thinking about how many ways employers can be fooled when designing a healthcare benefit plan. Specifically, how they can be fooled into thinking they’re making a high-value, cost-effective, transparently-priced primary care choice for their employees simply by choosing a model of primary care that calls itself “direct primary care.” It turns out, unfortunately, that not all who call themselves direct primary care actually create the kinds of clinical and financial outcomes employers believe come with the direct primary care label.
This benefits professional told me about a hospital system in his area that’s established a primary care practice they were calling direct primary care. Yet all referrals out of this practice were being funneled right back into the hospital system, the most expensive place in all of healthcare to have any test or procedure completed. This only makes sense from the hospital perspective because what hospitals really want from primary care is simply a direct channel of referrals. In fact, to hospitals, primary care is nothing more than “milk at the back of the store,” as Dave Chase likes to call it, placed there to get you to come inside and buy more expensive products.
This would, in fact, be a smart strategy for hospital systems to pursue if it were sustainable. Hospital systems understand there’s a movement by employers and forward-thinking benefits professionals to disrupt the status quo, to transform the payment model of primary care into one that incentivizes good outcomes rather than number of visits. Hospital systems can indeed provide immediate access to patients by shrinking the panel size of their so-called direct primary care physicians, just as happens in legitimate direct primary care practices. But then—unlike in legitimate direct primary care practices–they mandate that all downstream care take place in their system.
The problem, of course, is that their system is opaque and expensive. Direct primary care improves outcomes and reduces cost by avoiding unnecessary referrals into expensive hospital settings. For an employer to realize maximum health and financial benefits from adopting DPC into their health plan, it’s absolutely critical that the physicians not be incentivized or encouraged to refer to any provider that isn’t both high in quality and transparent in cost. Creating something called direct primary care that’s really just a subsidiary of a hospital system is equivalent to giving a fox the keys to the henhouse and asking him to guard it.
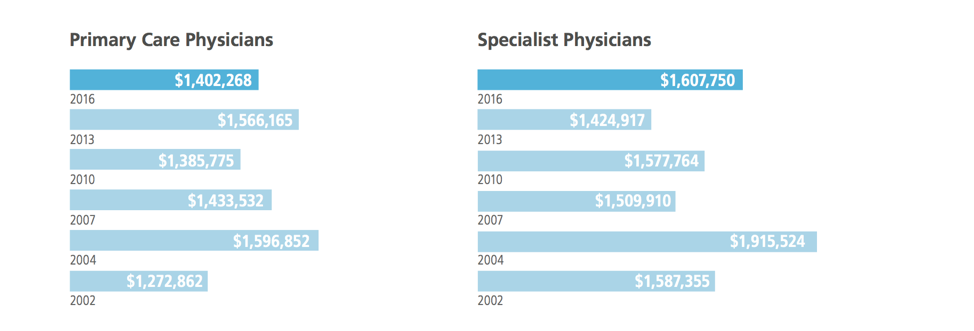
Direct primary care should never be constrained to refer only to the most expensive options for care. But direct primary care only makes sense for hospital systems to set up if it feeds patients into their machine. Data from Merritt Hawkins’ 2016 Physician Inpatient/Outpatient Revenue Survey show that in 2016 a primary care physician produced on average $1,404,268 dollars in downstream revenue for hospital systems. Specialist physicians, in contrast, produced on average $1,607,750. Interestingly, as you can see below, in one year, 2013, primary care physician downstream revenue actually surpassed specialist physician revenue.
The real value of direct primary care to hospital systems lies in the referrals direct primary care produces for them. But referrals to hospital systems are the most expensive of their kind and make authentic direct primary care look far less attractive to employers’ health plans than it actually is. Hospital systems looking to open their own direct primary care practices are simply jumping on the direct primary care bandwagon, working hard to hitch themselves to a movement that’s beginning to sweep the country. Change is coming, but beware the wolf in sheep’s clothing.
[jetpack_subscription_form title=” subscribe_text=’Sign up to get notified when a new blog post has been published.’ subscribe_button=’Sign Me Up’ show_subscribers_total=’0′]